Septoplasty in Turkey is a surgical procedure performed to correct deviations of the nasal septum that cause breathing difficulties. Prof. Dr. Murat Songu carries out this operation to restore normal airflow, offering patients a long-term solution for improved respiratory function and quality of life.
This procedure is often recommended for individuals suffering from chronic nasal obstruction, snoring, or recurrent sinus infections due to septal deviation. By straightening the septum, septoplasty enhances nasal airflow, reduces related symptoms, and improves overall well-being.
The cost of septoplasty in Turkey starts from 5,000 EURO, depending on the complexity of the septal deviation and patient-specific requirements. The fee generally includes consultation, anesthesia, surgical intervention, and structured post-operative care for safe recovery.
Recovery after septoplasty is usually quick, with most patients resuming daily activities within 7–10 days. Temporary swelling or congestion gradually subsides, and final functional results stabilize within a few months, providing lasting breathing improvement.

Turkey's Rhinoplasty Doctor
Prof. Dr. Murat Songu
Revision Rhinoplasty Specialist
Born in İzmir in 1976, Prof. Dr. Murat Songu entered İzmir Atatürk High School and then, in 1994, started at Ege University Faculty of Medicine. He completed his specialty training in Ear, Nose, and Throat Diseases at Celal Bayar University. In 2005, he worked on rhinology and otologic surgery in Bordeaux, France, at St. Augustin Clinic with Dr. Guy Lacher and at Bordeaux University with Prof. Vincent Darrouzet.
İçindekiler
One of the Best Surgeons for Septoplasty in Turkey
Prof. Dr. Murat Songu is recognized as one of the top surgeons for septoplasty in Turkey, correcting deviated septums with a focus on restoring unobstructed breathing. His ENT experience ensures precise internal adjustments with minimal impact on external nasal shape.
What Is Septoplasty and Why Is It Done?
The nasal septum is a cartilage‑and‑bone plate that runs from front to back and divides the nasal cavity into two separate tunnels. Because of congenital or acquired reasons, this structure can shift away from the midline. When the septum bends to the right or left, the condition is called “septal deviation” (simply, a deviated septum).
Septoplasty is the surgical procedure performed to correct this curvature. The main goal of the operation is to regulate airflow inside the nose, make breathing easier, and raise the patient’s day‑to‑day quality of life.
- Improved Breathing Quality: The airway narrowing caused by the curved septum is eliminated.
- Better Sleep Quality: Patients who snore or suffer from sleep apnea may experience relief.
- Fewer Chronic Sinusitis Attacks: Sinus ventilation and drainage become healthier.
The operation does not aim to create a dramatic change in outward appearance; it primarily straightens the inner curvature. Yet in some cases the deviation is so pronounced that the nose also looks crooked from the outside. When this happens, surgeons may plan aesthetic touches (rhinoplasty) in the same session.
Why Does the Nasal Septum Curve?
We call curvature of the nasal septum a “deviation.” Sometimes it is so mild that a person lives an entire life with no complaints; sometimes it causes marked shortness of breath that makes daily life difficult. So why does the septum curve?
- Congenital Structural Curvatures
Some people’s genetic code contains differences in nasal anatomy. Just as some of us have different leg lengths or hand‑foot shapes, the cartilage and bone structures inside the nose can vary. Even slight birth‑canal trauma during delivery can lead to septal curvature.
- Development‑Related Changes
During childhood and adolescence, bone and cartilage grow rapidly. If nasal and facial bones grow out of proportion, the septum is more likely to shift off‑center. For instance, if tissues on one side of the body do not develop in harmony with the other, they can slowly push the septum sideways.
- Trauma or Injury
Blows to the nose, traffic accidents, sports mishaps, or simple falls can easily displace the nasal bones. Sometimes this is noticed immediately; at other times it surfaces years later as “I can’t breathe.”
- Blows Especially in Childhood
In childhood the nose is still flexible. Even a mild bump when children fall can lay the groundwork for a hidden curvature in the nasal cartilage that may not be noticed until adolescence.
How Does a Deviated Septum Affect Everyday Life?
The nose works like an “air‑conditioning system”: it warms, humidifies, and filters the air we breathe. A curved septum can hinder these tasks. The main issues you might face are:
- Difficulty Breathing
Airflow from the narrowed nasal passage drops. Especially during exertion (climbing stairs or exercising), you may feel fatigued quickly.
- Habitual Mouth Breathing
People with chronic nasal congestion unknowingly begin to breathe through the mouth. This can cause throat dryness, bad breath, and gum problems.
Snoring and Sleep Problems
At night a blocked nose invites snoring. Breathing through the mouth instead of the nose can make the airways vibrate. Poor sleep quality may lead to daytime fatigue and difficulty concentrating.
- Susceptibility to Sinus Infections
For the sinuses around the nose to ventilate and drain properly, the nasal passages must be open. A curved septum can disrupt this natural drainage and lead to frequent sinus infections (sinusitis).
- Recurrent Nosebleeds
Airflow in a narrowed nasal channel can become turbulent, drying the nasal lining more easily. Dryness combined with minor irritation can cause bleeding.
As the severity of septal deviation increases, the frequency and intensity of these problems rise. Some people live for years saying, “I’m a bit congested, but it’s not a big deal.” Yet someone who can breathe comfortably through the mouth may actually be experiencing more serious symptoms. When nasal obstruction reaches the point where it affects the heart, lungs, or general health, treatment becomes essential.
Who Is a Good Candidate for Septoplasty?
Septoplasty is one of the main treatment options for people who suffer chronic breathing difficulty or related problems because of septal deviation. But not everyone with a deviated septum is a surgical candidate. Septoplasty is considered more seriously when:
- Inability to breathe or constantly sleeping with the mouth open disrupts daily comfort.
- Impaired sinus drainage causes chronic or recurrent sinusitis, and septoplasty may prevent this.
- Sleep apnea—breathing pauses during sleep—severely reduces quality of life, and nasal blockage worsens the picture.
- In some people the deviation is so pronounced it causes both functional and cosmetic problems; functional correction of the septum can be combined with aesthetic adjustments.
- Nasal decongestant sprays, corticosteroids, or antihistamines provide only temporary relief; if an underlying structural defect is the root problem, medication cannot offer a permanent solution.
Not every septal deviation requires surgery. Those with mild deviation and minimal complaints, or who respond to medication, may not need an operation. A medical examination is essential to determine candidacy. Endoscopic evaluation and, if necessary, imaging are performed, and the pros and cons are discussed before making a decision.
How Do You Prepare for Septoplasty?
As with any surgical procedure, there is a preparation phase before septoplasty. This is vital for boosting success and minimizing possible complications.
Medical Evaluation and Analysis
- A detailed examination of the nasal interior is conducted during the doctor visit.
- Breathing tests, endoscopic assessments, or, if needed, CT scans may be used.
- The patient’s overall health (heart, lungs, chronic diseases, etc.) is reviewed.
**Blood Tests and Routine Work‑ups**
- Pre‑op tests include complete blood count and clotting studies. They assess anesthesia suitability and predict intra‑operative complications.
**Medication Use and Extra Precautions**
- Blood‑thinning drugs may need to be stopped some time before surgery.
- No herbal supplements or vitamins should be taken without doctor approval; some increase bleeding tendency.
- Smokers are advised to quit at least a few weeks before surgery. Smoking adversely affects wound healing.
**Mental Preparation of the Patient**
- Patients may feel anxiety before any surgery. Talking openly with the doctor about concerns and learning what to expect helps reduce worry.
**Planning Additional Surgical Procedures**
- If the patient is also considering nasal aesthetics (rhinoplasty) or sinus surgery in the same session, planning is done accordingly. Other intranasal structures (turbinates, polyps, etc.) are checked and, if needed, a combined surgical plan is prepared.
Throughout preparation, close communication between doctor and patient is key. Discussing expectations, fears, and what might arise after surgery contributes to success both physically and psychologically.
How Is Septoplasty Performed?
Septoplasty aims to correct the curved cartilage and bone inside the nose. The general steps are:
Choice of Anesthesia
- General Anesthesia: The patient is fully asleep. Chosen if the operation will be long or for patient comfort.
- Local Anesthesia + Sedation: Suitable for certain simpler cases. The nose and surrounding area are numbed while the patient is lightly drowsy.
**Incision Site**
- A small incision is made inside the nose, usually leaving no visible scar. This allows access to the septum.
**Straightening the Septum**
- Accessing Cartilage and Bone: The mucosal lining (mucoperichondrium) is carefully lifted.
- Reshaping or Removing Curved Sections: Deviated cartilage pieces can be cut, reshaped, or completely removed. The goal is to preserve as much tissue as possible to maintain nasal support.
- Centering the Septum: After corrections, the septum is stabilized near the midline.
**Closing Tissue and Incision**
- The lifted mucosa is repositioned.
- Special suturing techniques, splints, or stents may be used if the surgeon deems fit. These help keep the septum in place.
- Tampon packing is rarely needed. Modern methods often suffice with gentle support or special adhesives, avoiding the discomfort of traditional packs.
**Additional Procedures**
- If turbinate reduction or sinus cleaning is needed, these are done at this stage. Total surgery time ranges from 30 minutes to several hours depending on scope.
- Septoplasty can be performed with microscopic or endoscopic tools. Modern techniques provide better visualization, increasing precision and shortening recovery.
What Should You Watch Out for After Surgery?
Recovery after septoplasty is generally comfortable, but several points deserve attention:
Rest and Sleep Position
- For the first few days, keep the head slightly elevated while lying down (e.g., with an extra pillow) to improve circulation and reduce swelling and bleeding risks.
**Nasal Care**
- Saline Sprays: Keep the nasal interior moist and prevent crusting.
- Gentle Cleaning: Never wipe the nose harshly or blow forcefully.
- Prescribed Medications: Antibiotic ointments or drops may be given; using them regularly speeds healing.
**Pain Management**
- Most patients experience mild‑to‑moderate pain, controllable with the prescribed analgesics. Avoid aspirin or certain blood‑thinning painkillers.
**Physical Activity**
- Avoid heavy exercise and movements that require bending the head forward during the first week.
- Stay away from contact sports or activities with a risk of impact for about two weeks. The nose is more vulnerable while healing.
**Follow‑up Visits**
- Attend scheduled check‑ups to have sutures or splints removed at the right time and detect complications early.
**Nutrition**
- After surgery, choose soft foods that are neither very hot nor very cold. Extremely spicy foods can irritate the nose and throat. Plenty of fluids support overall healing.
Most swelling and crusting inside the nose subside within one to two weeks. Full healing can take several months. Strictly following the doctor’s instructions minimizes complications and boosts success.
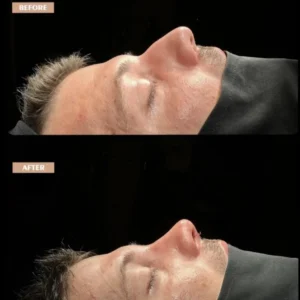
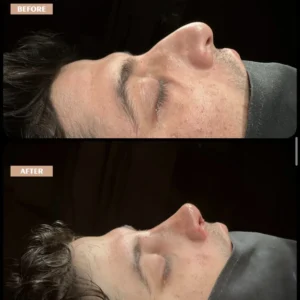
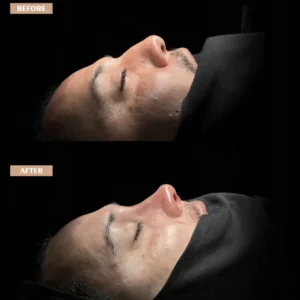
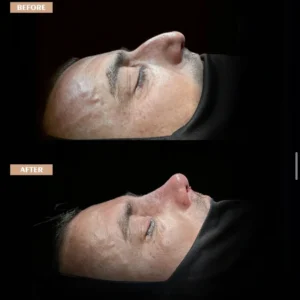
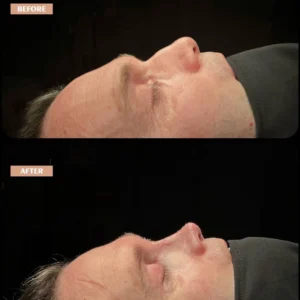
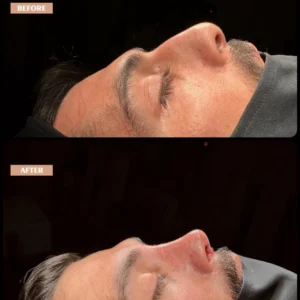
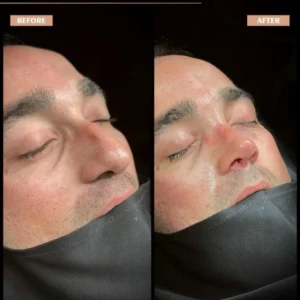
Before & After Gallery
What Are the Expectations and Recovery Timeline After Septoplasty?
Most patients have a smooth recovery and notice significant breathing improvement over time, though full results can take months. Keeping expectations realistic helps:
Symptoms in the First Days
- A feeling of fullness and pressure inside the nose is normal.
- Minor bloody discharge, especially in the first 24–48 hours, is common.
- Mild facial bruising or swelling is rare and usually occurs only when additional procedures are performed.
**Gradual Breathing Improvement**
- Nasal congestion starts to ease in the first week, but mucosal swelling may delay full relief.
- Marked airway opening is usually felt after about 2–3 weeks.
- Final results emerge in 3–6 months.
**Return to Daily Life**
- Desk work or other light duties can usually be resumed in 3–5 days.
- Wait for doctor approval before heavy physical labor or intense exercise.
**Changes in the Senses**
- Some patients temporarily notice reduced smell or taste.
- This generally resolves as healing progresses.
**Check‑ups and Follow‑up**
- Regular visits let the doctor clean crusts and monitor healing. If adhesions form, they can be treated early.
Expecting an immediate “miracle breath” right after surgery is unrealistic. Yet with patience and adherence to guidance, breathing becomes noticeably clearer day by day, and the long‑term quality‑of‑life gains reveal the procedure’s value.
Possible Side Effects and Complications
Like all surgeries, septoplasty carries risks, though rates are low and most issues are manageable. Potential side effects include:
Bleeding (Epistaxis)
Light oozing is normal in the first days. Rarely, heavy bleeding may require medical attention.
- Infection
Though uncommon, intranasal infections may need antibiotics. Regular dressings and care reduce this risk.
- Septal Hematoma
Blood may collect between the two sides of the septum. Untreated, it can compromise cartilage nutrition and cause serious problems. It is easily detected during follow‑ups and resolved by drainage.
- Septal Perforation (Hole)
Rarely, a small hole can form in the septum during or after surgery. This may cause dry airflow, crusting, or minor bleeding. Corrective surgery can be done later if necessary.
- Adhesions (Synechiae)
Healing tissues may stick together in the wrong place. If they obstruct breathing, a minor procedure can separate them.
- Persistent Breathing Issues
Some patients do not feel complete relief. Enlarged turbinates, polyps, or allergic rhinitis may be responsible; further treatment can help.
- Possible Cosmetic Changes
Interfering with septal support can rarely cause a saddle‑nose deformity or shape change. Preserving adequate cartilage minimizes this risk.
Despite these possibilities, septoplasty is very safe and successful when properly indicated and performed by experienced hands. Diligent pre‑ and postoperative care by the patient greatly reduces complications.
Can Other Procedures Be Done Together With Septoplasty?
Septoplasty is often performed alone but sometimes combined with other nasal or sinus surgeries:
- Turbinate Reduction (Turbinoplasty or Turbinectomy)
If the turbinates are enlarged and blocking airflow, their size can be reduced simultaneously, giving more effective relief.
- Sinus Surgery (Endoscopic Sinus Surgery)
In chronic sinusitis or when polyps are present, sinus pathways can be opened in the same session—one anesthesia, one recovery.
- Rhinoplasty (Cosmetic Nose Surgery)
Patients unhappy with nose shape or with structural issues affecting function can have rhinoplasty along with septoplasty (septorhinoplasty), correcting both internal and external problems in one go.
- Removal of Nasal Polyps
Polyps arising from allergies or chronic sinusitis can be surgically removed at the same time.
Combined operations mean one anesthesia and one recovery period, but surgery time is longer and follow‑up must be more meticulous. The decision is tailored to each patient.
The best path for a worried patient is to consult a specialist and ask every question. Turning fears into concrete information makes the journey manageable.
What Is the Success Rate of Septoplasty?
Success is measured mainly by how well the operation restores comfortable nasal airflow. Proper patient selection, surgeon experience, surgical technique, and adherence to postoperative care all influence results.
- Improved Breathing: Most patients report noticeably easier breathing.
- Reduced Sinus and Snoring Issues: Sinus infections and snoring often decline.
- Need for Revision Surgery: Rarely, optimal improvement is not achieved or new deviations develop, but this occurs in a small minority.
No surgical procedure offers a 100 % guarantee, yet septoplasty is widely regarded as an effective, safe method for correcting functional nasal problems. Good timing, meticulous planning, and strict adherence to postoperative advice maximize success.
Are Septoplasty Results Permanent in the Long Term?
The effects of septoplasty are largely permanent once healing is complete, but exceptions exist:
- Strong blows or accidents can re‑deviate the septum.
- Rarely, ongoing cartilage and bone remodeling can partly recur curvature.
- Allergies, polyps, or turbinate enlargement can re‑cause nasal blockage; the issue then is not septal deviation but another structural or inflammatory process.
- Aging changes bones, cartilage, and soft tissues over time, but these usually do not negate the operation’s benefits.
Thus septoplasty is designed to be a lifelong solution. Protecting the nose from trauma and having regular check‑ups for other airway problems help maintain long‑term success.
What Is the Link Between a Deviated Septum and Allergic Rhinitis?
Allergic rhinitis is an over‑reaction of the nasal mucosa to allergens like pollen, dust, or animal dander, causing swelling, discharge, sneezing, and itching. While septal deviation and allergic rhinitis are not directly cause‑and‑effect, they influence each other:
- Airway narrowing from a curved septum, combined with mucosal swelling during an allergic reaction, makes breathing far harder.
- Medication (antihistamines, steroid sprays) is first‑line for allergies, but if deviation persists and meds fall short, correcting airflow with septoplasty can boost drug effectiveness.
- In allergic patients, controlling allergy and reducing swelling before surgery is advised; operating during an active flare can hamper healing.
- Controlling allergies post‑op also reduces mucosal reactions, helping maintain results.
Together, allergic rhinitis and septal deviation can markedly impair nasal airflow; treatment is planned with a multidisciplinary approach.
Should I Be Afraid of Having Septoplasty?
Thinking about surgery can evoke anxiety, yet modern medicine offers very safe, comfortable methods for functional nasal surgery like septoplasty. Points that can ease fears:
- Experienced surgeons and anesthesia teams raise success and reduce risks.
- Talking through the process, the procedure, and the recovery demystifies the unknown.
- General anesthesia eliminates pain and awareness; local anesthesia + sedation is also safe for select cases.
- Most people return to everyday life in 1–2 weeks. With splint‑only or pack‑free techniques, discomfort is far less than in the past.
- Bleeding, infection, and other complications are rare and manageable when they do arise.
- A lifetime of easier breathing, better sleep, and fewer sinus attacks usually outweighs the initial anxiety.
Will My Nose Shape Change After Septoplasty?
Septoplasty is primarily functional, aiming to correct the internal septum; the external nose is not usually targeted. However, note:
- Because the septum supports the nasal bridge and tip, correcting a severe deviation may subtly straighten the outer nose—a natural, often welcome symmetry.
- When esthetic and functional issues are treated together, septoplasty plus rhinoplasty (septorhinoplasty) is performed, intentionally altering the external appearance.
- Removing too much cartilage can cause a collapsed or crooked look. Skilled surgeons remove only what is necessary and preserve support.
- Protecting the nose from trauma post‑op is vital; direct blows or heavy pressure can shift bones and cartilage before they set.
Early swelling may make the nose look slightly different; this is temporary. Over a few months the true, usually satisfying, shape becomes apparent if no cosmetic change was planned.
Will My Nasal Blockage Disappear Completely After Septoplasty?
Septoplasty tackles one of the most important structural causes of nasal obstruction—septal deviation—so significant relief is expected, but:
- Additional issues such as allergic rhinitis, turbinate hypertrophy, polyps, or sinus problems also need treatment for complete relief.
- Obesity, smoking, or hypertension can affect tissue healing, causing temporary blockage.
- Insufficient care may lead to crusting or adhesions, creating new obstruction; regular follow‑ups curb this risk.
- Swelling and crusting can partly block the nose for the first weeks; this is a transient phase.
Septoplasty is among the most effective surgical interventions for nasal congestion, but healing takes time, and realistic expectations matter. Most people feel discernible breathing ease from the early weeks onward, which increases as recovery advances.
How Does Septoplasty Affect Quality of Life?
Many think the nose serves only to breathe, but breathing quality affects quality of life in multiple ways. Expected changes after septoplasty include:
- Deeper, easier breathing improves blood oxygen, boosting energy and daily performance.
- Reduced nasal blockage alleviates snoring or sleep apnea, enabling uninterrupted, restorative sleep.
- Not constantly sniffing or walking around with the mouth open lifts self‑confidence and social comfort.
- Steady breathing eases cardiovascular strain; better sinus ventilation decreases sinusitis frequency, benefiting overall health.
Though primarily a “breathing” operation, septoplasty’s effects extend far beyond airflow, enhancing daily life, sleep, social interactions, and even mental well‑being—especially in patients with significant deviation whose improvement can be striking.