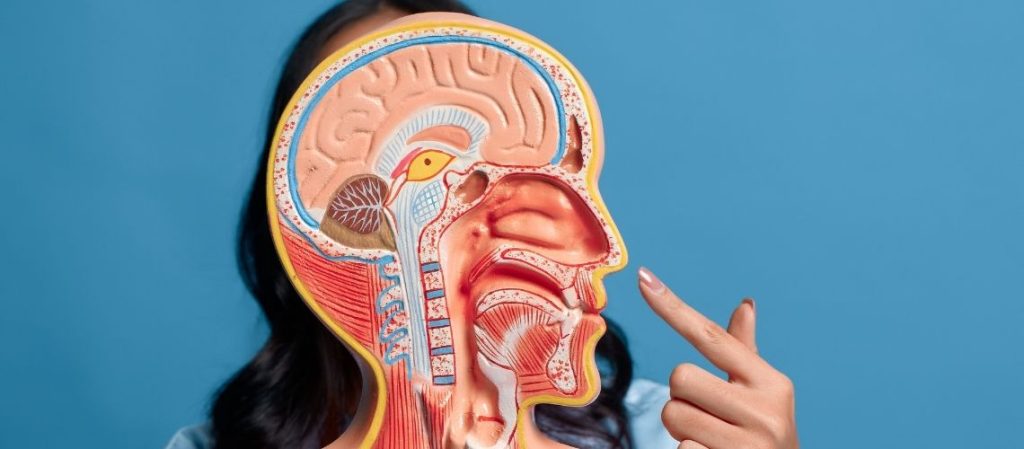
Nasal anatomy consists of bones, cartilage, muscles, and mucosa, which together shape the nose and its functions. Understanding these structures is crucial for both medical and aesthetic interventions.
The upper portion of the nose is supported by nasal bones, while the lower part is primarily cartilaginous. This combination determines stability and flexibility.
The nasal cavity is lined with mucosa that filters, warms, and humidifies inhaled air. This protective system supports healthy respiratory function.
Detailed knowledge of nasal anatomy allows surgeons to perform precise interventions. Balancing form and function ensures safe and aesthetic outcomes.
İçindekiler
What Are the Main Structures in Nasal Anatomy?
Nasal anatomy comprises several key structures that ensure the functional and structural integrity of the nose. These include the external nose, the nasal septum, the nasal cavity, and the nasal cartilages. The external nose consists of both bony and cartilaginous components: the bony part includes the nasal bones and the frontal process of the maxilla, while the cartilaginous part contains various cartilages that give flexibility to the nose. Main structures in nasal anatomy include:
- Nasal root
- Dorsum (bridge)
- Apex (tip)
- Nares (nostrils)
The nasal septum divides the nasal cavity into two and provides support to the nose. Made up of bony and cartilaginous sections, this structure regulates airflow while contributing to the stability of the nose. Deviations can affect the septum’s function, creating problems in airflow. The nasal cavity is located behind the external nose and is divided into two halves by the septum. With the protrusions of the turbinates (which increase surface area), the mucosal layer inside the cavity traps particles and humidifies the air. The paranasal sinuses connect to the nasal cavity, contributing to voice resonance.
Nasal cartilage preserves the external and structural shape of the nose. The cartilages responsible for shaping the nostrils and supporting the septum provide flexibility, aiding in shock absorption. The functionality of these fundamental structures directly affects the nose’s breathing and olfactory capabilities and helps maintain nasal health.
How Does the Nasal Cavity Support Breathing?
The nasal cavity supports bodily health by conditioning the air during respiration. Air entering through the nostrils is cleaned, warmed, and humidified by various structures in this region. Thus, inhaled air reaches the lungs under ideal conditions, protecting the delicate tissues of the respiratory tract. The main structures in the nasal cavity that support breathing are:
- Nasal hairs
- Turbinates (conchae)
- Ciliated pseudostratified epithelium
- Goblet cells
- Olfactory region
The air undergoes turbulence within the nasal cavity due to the turbinates, remaining in contact with the mucosa for a longer period. This allows the air to be sufficiently warmed and humidified, facilitating its safe passage to the lungs. Additionally, some of the air is directed to the olfactory region, enabling the sense of smell.
What Is the Role of the Nasal Septum in Nasal Function?
The nasal septum splits the nasal cavity into two, ensuring balanced airflow through both nasal passages. This structure regulates how inhaled air circulates within the nose, contributing to the effective operation of various protective mechanisms. The septum’s natural midline position supports the nasal cycle, in which nasal blockage and openness alternate rhythmically, optimizing the efficiency of nasal function. It is also known that by expanding the internal nasal surface, the septum helps humidify and warm the air.
Main functions:
- Balancing airflow
- Regulating air circulation during breathing
- Aiding in air humidification
- Filtering dust and particles for protection
- Facilitating the direction of odors toward the olfactory epithelium
Deviations in the nasal septum’s structure, especially in what is known as a deviated septum, can weaken these protective and regulatory functions. A crooked septum can lead to nasal congestion, dry mouth, and sinus blockage; in more severe cases, it may trigger snoring and sleep disorders. Such anatomical irregularities can affect the overall respiratory system health by reducing both the quantity and the quality of inhaled air. Surgical interventions such as septoplasty may be necessary to lessen the impact of septal deviations and restore nasal function.
How Do Turbinates (Nasal Conchae) Affect Airflow?
Turbinates are bony structures within the nasal cavity that regulate airflow. Owing to their specific arrangement and functions, the inhaled air is guided through narrow passages, slowing the airflow and increasing its contact with the mucosal surface. This mechanism ensures that inhaled air is brought to an optimal state before reaching the lower airways. The turbinates’ roles in promoting healthy airflow in the nose include:
- Slowing down the speed
- Warming
- Humidifying
- Partially filtering
The turbinates also create turbulence to further improve the quality of the air entering the respiratory tract. This turbulence increases the contact between particle-laden air and the mucus layers, aiding in trapping allergens and particles. Thanks to vascular erectile tissue, the size of the turbinates can change, allowing the airway resistance to adapt to respiratory needs and helping maintain a balance against nasal congestion.
What Is the Function of the Nasal Vestibule (Nasal Entrance)?
The nasal vestibule lies just behind the nostrils and forms the first line of defense in the respiratory tract. Its primary function is to capture large particles in inhaled air, keeping the airways clean. The stratified squamous epithelial layer makes the vestibule resistant to environmental factors. Embedded within this epithelial layer are protective hairs that effectively trap dust and larger particles, preventing them from moving deeper into the airways. The key functions of the nasal vestibule include:
- Large particles
- Dust
- Airborne debris
Additionally, the sebaceous glands in the nasal vestibule combine with mucus to form a moist layer that aids in trapping foreign matter within the nose. The mucosal coating over these protective hairs not only filters the air but also helps to humidify and soften the inhaled air. These features protect the sensitive structures of the respiratory system from external factors while reducing the irritating effect of incoming air.
These defensive mechanisms in the nasal vestibule ensure that the inhaled air transitions into the nasal cavity in a clean and safe manner, decreasing the amount of particles that reach the lungs and supporting respiratory health.
How Does the Sense of Smell Occur in the Nose?
The sense of smell begins in the olfactory epithelium located in the nose, and is completed through complex interactions between the nose and various regions of the brain. Odor molecules initially adhere to the mucus in the upper part of the nasal cavity where the olfactory epithelium is found. Dissolved in the mucus, these odor molecules come into contact with receptor neurons within the epithelium. Each neuron carries receptors that respond to the specific molecular structures of odors, enabling the perception of a wide range of smells.
Olfactory processing occurs in three main steps:
- The olfactory epithelium, filled with fine sensory receptors
- The cribriform plate, which carries odor signals to the brain
- The olfactory center, which identifies and organizes odor signals
The signals processed in the olfactory center are transmitted via the olfactory pathway to the cerebral cortex and the limbic system, linking smells with memory and emotion. Structures in the limbic system, such as the amygdala and the hippocampus, play crucial roles in forming emotional responses to odors and in reactivating memories.
The sense of smell operates through two different pathways: the orthonasal pathway for odors inhaled through the nose and the retronasal pathway for aromas originating from foods in the mouth. The combination of smell and taste perception enriches the flavor of foods and the overall consumer experience. This multifaceted system makes humans sensitive to the broad variety of odors in their environment and enables rapid responses to environmental stimuli.
Why Are Humidification and Filtration Important in Nasal Breathing?
Humidification and filtration processes in nasal breathing support the healthy functioning of the respiratory system. Air taken in through the nose is brought to an appropriate temperature and humidity level before it reaches the lungs. These processes occur thanks to the mucosal membranes in the nasal cavity and the nasal turbinates, ensuring that the air is in a condition that does not harm the sensitive tissues of the lungs.
During this process, the nose:
- Brings the air temperature close to 37°C (98.6°F)
- Increases humidity to nearly 100%
- Draws moisture from the mucus layer
- Creates turbulence to enhance contact with the mucosa
- Protects the respiratory tract from pollutants
Additionally, breathing through the nose involves a filtration process carried out by nasal hairs and cilia that capture pathogens and particles. This filtration prevents harmful substances from reaching the lower airways, reducing the burden on the immune system. Another significant effect of filtration is the increase in nitric oxide release during nasal breathing; this compound has antimicrobial properties and helps neutralize microbes present in inhaled air.
The nose also provides protection against irritants in the air, which improves gas exchange efficiency in the lungs and reduces the risk of inflammation in the respiratory tract. Nasal breathing is therefore crucial for optimal respiratory function and overall health.
How Does the Nasal Cavity Contribute to Immunity?
The nasal cavity serves as the first line of defense for the immune system through its role in maintaining respiratory tract health. Cilia and mucus form an effective barrier in the nose, preventing pathogens, allergens, and harmful particles from entering the respiratory passages. Cilia move rhythmically to push mucus toward the throat, where trapped particles are expelled from the body. The mucus layer contains high levels of mucins and antimicrobial peptides, which hinder pathogens from adhering to the nasal epithelium.
- Ciliary function
- Mucus structure
- Types of mucin: MUC5AC, MUC5B
- Antimicrobial components
- Ion channels
The viscosity and hydration of the mucus layer are regulated by ion channels, creating an effective barrier against pathogens. Ion transport increases mucus fluidity, optimizing nasal defenses. Cilia continuously move the mucus, clearing the nasal cavity and minimizing the risk of pathogens reaching the lower airways. This system integrates with immune cells and secretory immunoglobulins (like IgA) to neutralize microorganisms that might evade the mucociliary defense.
What Are Paranasal Sinuses and How Do They Support Nasal Structure?
The paranasal sinuses are air-filled cavities within the cranial bones surrounding the nasal cavity. These structures, which help support functions such as head balance and voice quality, complete the nasal architecture. One of the primary roles of the sinuses is to reduce the weight of the skull. Being filled with air, the skull requires less muscular support, placing less strain on the neck muscles. This promotes more comfortable head movement and contributes to energy conservation, while also helping maintain balanced cervical spine posture. The paranasal sinuses are located in different bones that support the nasal structure from various angles, including:
- Frontal bone
- Ethmoid bone
- Sphenoid bone
- Maxillary bone
Another significant function of the paranasal sinuses is providing resonance for the voice. These chambers assist in amplifying sound waves, giving each individual a unique vocal timbre. Differences in the size and shape of the sinuses can lead to variations in voice characteristics among individuals, thus playing a key role in speech and voice modulation.
The sinuses also contribute to respiratory health through mucus production. Lined with mucosal membranes, these structures direct mucus flow toward the nose and protect the nasal cavity. This mucus traps dust and pathogens in the air, preventing them from reaching the lungs, and also helps to humidify the nasal passages. When the sinuses become blocked, mucus flow is disrupted, leading to inflammation and breathing problems. In this way, the paranasal sinuses protect the nose and the overall respiratory system, supporting healthy breathing.
What Common Conditions Affect Nasal Function?
Common conditions that affect nasal function can cause significant changes in nasal anatomy and physiology, negatively impacting breathing quality and the sense of smell. These conditions include rhinitis, sinusitis, and nasal polyps. Rhinitis is characterized by inflammation of the nasal mucosa and is divided into allergic and non-allergic types. In allergic rhinitis, environmental allergens such as pollen or dust mites trigger the immune system to release histamine, leading to various symptoms. Non-allergic rhinitis, however, is triggered by external factors without an immune response. Common symptoms of these conditions include:
- Sneezing
- Nasal congestion
- Runny nose
- Itching
Sinusitis develops when the sinus cavities around the nose become inflamed. Acute sinusitis is usually viral in origin, while chronic sinusitis may develop from ongoing bacterial infections, fungi, or untreated allergies. Symptoms of sinusitis include:
- Facial pain
- Pressure sensation
- Thick nasal discharge
- Reduced sense of smell
Nasal polyps are benign growths that develop as a result of chronic inflammation in the nose and sinuses. They are more common in individuals with chronic sinusitis, asthma, or aspirin sensitivity. Polyps block sinus drainage and restrict nasal airflow. The primary symptoms caused by nasal polyps include:
- Nasal obstruction
- Postnasal drip
- Facial pressure
- Reduced sense of smell
As nasal polyps grow or multiply, they further limit airflow in the nasal cavity, exacerbating chronic sinusitis symptoms.

Prof. Dr. Murat Songu – Rhinoplasty (Nose Aesthetics) Specialist
Prof. Dr. Murat Songu was born in 1976 in Izmir and completed his medical education at the Ege University Faculty of Medicine. He then completed his residency training in the Department of Otorhinolaryngology at Celal Bayar University. Between 2005 and 2006, he received advanced training in rhinoplasty, functional nasal surgery, and skull base surgery in Bordeaux, France, working with leading rhinologists such as Prof. Vincent Darrouzet and Dr. Guy Lacher.
Prioritizing natural appearance, the preservation of breathing function, and facial aesthetic harmony, Prof. Dr. Songu is nationally and internationally recognized for his expertise in open rhinoplasty, piezo (ultrasonic) rhinoplasty, revision rhinoplasty, tipplasty, and functional septorhinoplasty. He has participated as an instructor and speaker at numerous rhinoplasty congresses worldwide.
With over 100 scientific publications, book chapters, and more than 1700 citations, Prof. Dr. Murat Songu is one of Türkiye’s most respected academics in the field of rhinoplasty, combining natural, facially harmonious, and functional results with scientific and aesthetic excellence.